Can Ticks Make You Allergic to Beef?
The idea that a tick bite could lead to a food allergy may sound like something out of a science fiction novel, but it is a reality for some individuals.
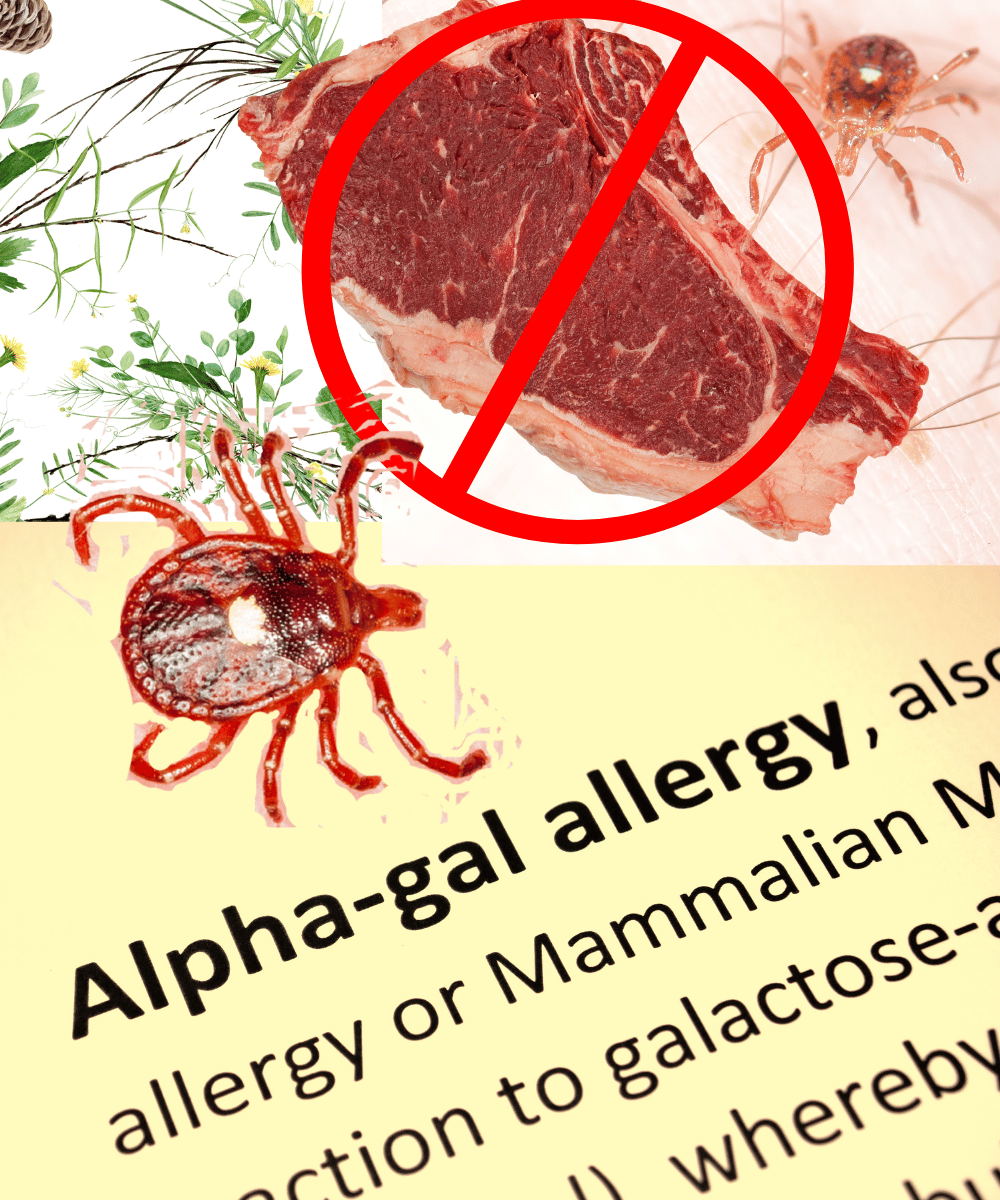
In recent years, a peculiar link between tick bites and allergies has emerged, leaving many to wonder about the connection between these tiny creatures and our dietary habits. Specifically, the question arises: Can ticks make you allergic to beef? This article delves into the science behind this phenomenon, exploring how a bite from a certain type of tick can lead to an unexpected and potentially life-changing allergy to red meat.
Key Takeaways:
- Ticks can cause a meat allergy known as Alpha-gal syndrome (AGS).
- The Lone Star tick is primarily responsible for transmitting the allergy-inducing molecule.
- Awareness and prevention are key to managing the risk of developing AGS.
The Science Behind the Bite
The idea that a tick bite could lead to a food allergy may sound like something out of a science fiction novel, but it is a reality for some individuals. The condition is known as Alpha-gal syndrome (AGS), and it is triggered by the bite of certain species of ticks. When these ticks feed on humans, they can transmit a sugar molecule called alpha-gal into the person's bloodstream. This molecule is not naturally found in humans, but it is present in the meat of mammals such as cows, pigs, and lamb.
For reasons not entirely understood, the immune system of some people who are bitten by these ticks begins to produce antibodies against alpha-gal. Once this immune response is established, consuming red meat can trigger an allergic reaction, as the body now recognizes the alpha-gal in the meat as a threat.

The Culprit: Lone Star Tick
The primary vector for this allergy is the Lone Star tick, named for the single white spot on the female's back. Found predominantly in the southeastern United States, the Lone Star tick has been spreading northward and westward, potentially increasing the incidence of AGS. It's not just the Lone Star tick, though; other tick species around the world have also been implicated in the transmission of the alpha-gal molecule.
When a Lone Star tick bites a human, it is not the tick itself that causes the allergy but rather the alpha-gal molecule that it transmits from its previous animal host. This molecule is foreign to the human body, which can prompt the immune system to react defensively upon future exposure to alpha-gal in meat.
Identifying Alpha-gal Syndrome
Recognizing AGS can be challenging because the symptoms can vary widely among individuals and may not appear immediately after consuming red meat. Common reactions include hives, itching, stomach pain, and in severe cases, anaphylaxis. What makes AGS particularly tricky is that the allergic reaction can occur several hours after eating, which is atypical for most food allergies.
To diagnose AGS, healthcare providers rely on a combination of the patient's history of tick bites, symptoms, and blood tests that can detect antibodies to alpha-gal. Once diagnosed, the treatment for AGS primarily involves avoidance of red meat and products containing alpha-gal.
The Impact of Diet on AGS
For those diagnosed with AGS, dietary changes are necessary to prevent allergic reactions. This means avoiding all mammalian meats and products derived from mammals, such as gelatin, which can be found in many processed foods and medications. Adapting to a diet free of these products can be challenging and requires careful label reading and, in some cases, dietary counseling.
Despite the restrictions, individuals with AGS can still enjoy a varied diet. Poultry, fish, and plant-based proteins are safe alternatives that provide necessary nutrients without the risk of an allergic reaction. With the growing popularity of vegetarian and vegan diets, there are more options than ever for those needing to avoid red meat.
Prevention and Awareness
The best way to prevent AGS is to avoid tick bites. This involves using insect repellents, wearing protective clothing, and performing thorough tick checks after spending time outdoors, especially in areas known to have a high tick population. Public awareness campaigns are crucial in educating people about the risks of tick bites and the potential for developing AGS.
Healthcare professionals also play a vital role in prevention by staying informed about the signs and symptoms of AGS and considering it as a potential diagnosis for patients presenting with unexplained allergic reactions. Early diagnosis can prevent severe reactions and improve the quality of life for those affected.
Living with Alpha-gal Syndrome
Living with AGS requires a significant lifestyle adjustment, but it is manageable with the right support and resources. Individuals with AGS must be vigilant about their food choices and aware of the potential for cross-contamination. Eating out can be particularly challenging, as it requires clear communication with restaurant staff about the allergy.
Support groups and online communities can provide valuable information and emotional support for those adjusting to life with AGS. Sharing experiences and tips can make the transition to an alpha-gal-free diet easier and less isolating.
The Role of Research
Ongoing research is crucial to understanding AGS better and finding potential treatments. Scientists are investigating why only some people develop the allergy after a tick bite and what factors may predispose an individual to AGS. There is also interest in developing therapies that could desensitize people to alpha-gal, much like allergy shots for other types of allergies.
As the range of the Lone Star tick and other tick species continues to expand, research into AGS will become increasingly important. Understanding the mechanisms behind the allergy and how to prevent it can help reduce the incidence and impact of AGS.
The Global Perspective
While AGS is most commonly associated with the Lone Star tick in the United States, similar allergies have been reported worldwide. Ticks in Europe, Australia, and Asia have also been found to transmit the alpha-gal molecule, leading to cases of meat allergy in these regions.
This global occurrence underscores the need for international collaboration in research and awareness efforts. Sharing knowledge and resources can help improve prevention strategies and treatment options for those affected by AGS around the world.
The Future of AGS Management
As awareness of AGS grows, so does the potential for better management and treatment options. The development of new diagnostic tools and therapies could significantly improve the lives of those with the allergy. Additionally, changes in land use and wildlife management may influence tick populations and, consequently, the prevalence of AGS.
The future of AGS management lies in a combination of public health initiatives, medical advancements, and individual awareness and prevention strategies. By working together, we can reduce the risk and impact of this unusual but increasingly common allergy.
Summary
Alpha-gal syndrome is a tick-induced allergy to red meat that has been gaining attention due to its unusual nature and the increasing range of the ticks responsible for its transmission. The Lone Star tick is the primary culprit in the United States, but similar allergies have been reported globally. Diagnosis involves a combination of patient history, symptom recognition, and blood tests. Management of AGS requires dietary changes and vigilance to avoid exposure to alpha-gal. Prevention is key, and ongoing research is essential to improve understanding and treatment of this condition.
FAQ Section
Q: Can any tick bite lead to a meat allergy? A: No, not all tick species are capable of transmitting the alpha-gal molecule. The Lone Star tick is the primary vector in the United States, but other species in different parts of the world have also been implicated.
Q: How long after a tick bite can AGS symptoms appear? A: The development of AGS symptoms can vary. Some individuals may experience reactions within a few weeks of the tick bite, while others may not develop symptoms for several months.
Q: Is there a cure for Alpha-gal syndrome? A: Currently, there is no cure for AGS. The primary treatment is strict avoidance of red meat and other products containing alpha-gal. Research is ongoing to find potential treatments and to understand why some people develop the allergy while others do not.
